My Loved One’s Breaking Our Agreement About Use at Home. What Should I Do About It?

Photo credit: Stevano Vicigor
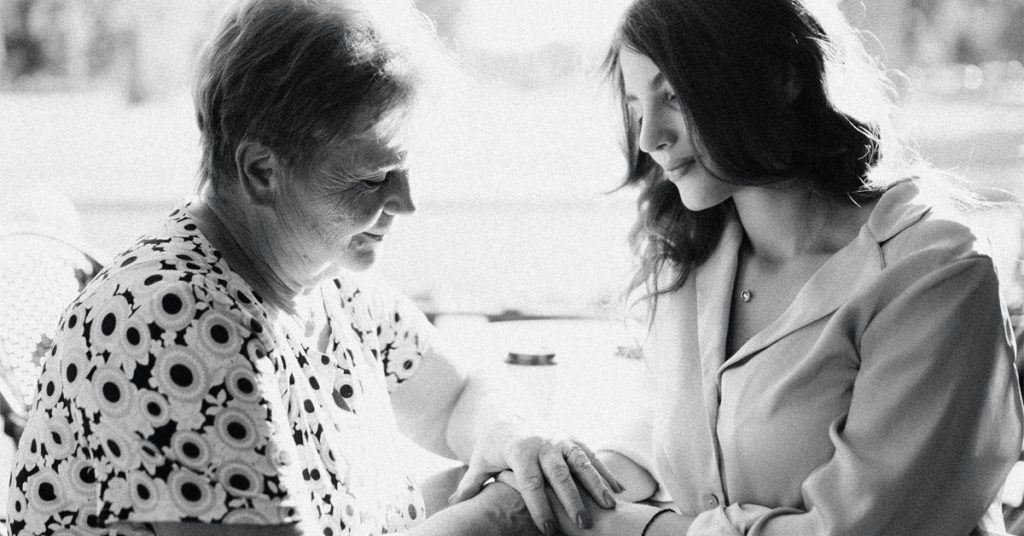
After time in a recovery house—and agreeing in writing not to use while living at home— a member’s Loved One has moved in with her. Much has been going well, but now the accumulating signs leave little doubt: they’re using again. She has been working hard to apply CRAFT to her situation. She worries, though, that her “watchful silence” might be counterproductive. Laurie MacDougall brings her back to a key, if difficult, CRAFT fundamental: boundary setting.
My 25-year-old Loved One is in early recovery. They moved home recently from a recovery house, and we came to a written agreement, which includes no use while living at home. Things are going well on many levels: they have a steady job, are going to meetings, have a sponsor, have picked up former hobbies, and seem to want to build a community of support.
But I’ve seen a change of pattern over the past four weeks that suggests they’re using. They hide it well, are very high functioning. But at this point, all the small clues are adding up: blood spots, soot, spoons in the bathroom, not taking suboxone as prescribed, etc. I’ve had a couple of productive CRAFTy conversations with them where I’ve shared concerns, but they have not acknowledged use. They overdosed several years ago at home and barely survived.
While I’m practicing CRAFT by leaning in when they are not using and removing myself when they are, it has been hard. And at this point I feel like my watchful silence is somehow enabling use. I’m starting to feel anxious and increasingly concerned. Thoughts?
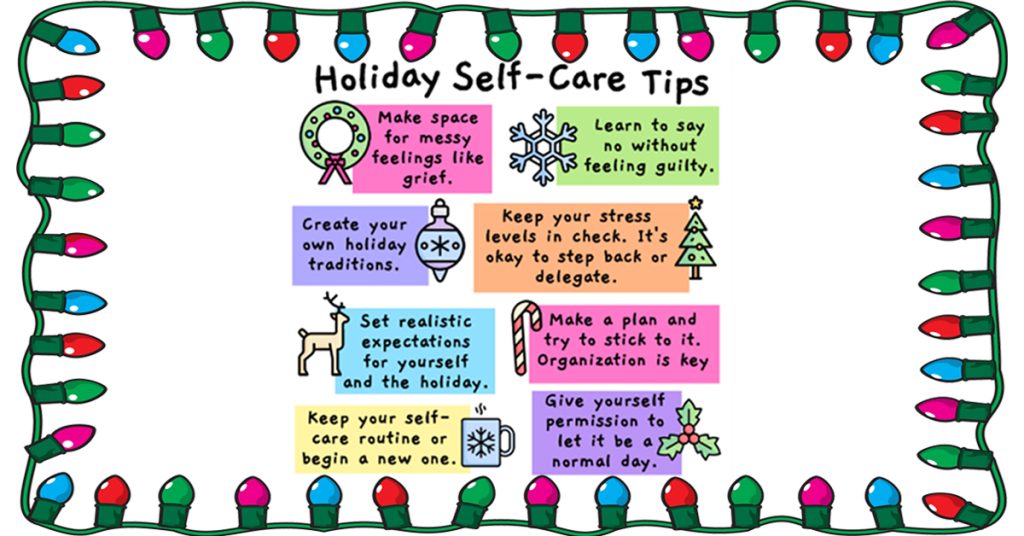
I have found that one of the most misunderstood CRAFT concepts is boundaries. There are a couple of aspects of boundaries that are key to pulling them off. I bring this up at the start because I suspect there a couple of things that have to happen to make your agreement effective.
It sounds like your LO has experienced both progress and setbacks at the same time. I would encourage you to continue to reward any positive steps that your LO has made or is making, while at the same time addressing the difficult and challenging issue of use while living at home. That use is not only dangerous; it’s crossing a boundary everyone agreed upon.
Let me pose a few initial questions. What did you both agree would happen if there was use in your house? And do you really need your Loved One (LO) to admit to use in order to follow through? Are you thinking that maybe if your LO admits to use, they will be accepting and more compliant of the action steps agreed to? And/or are you hoping that if they admit to it, they won’t be upset or act in ways that spiral out of control?
You already know what’s happening
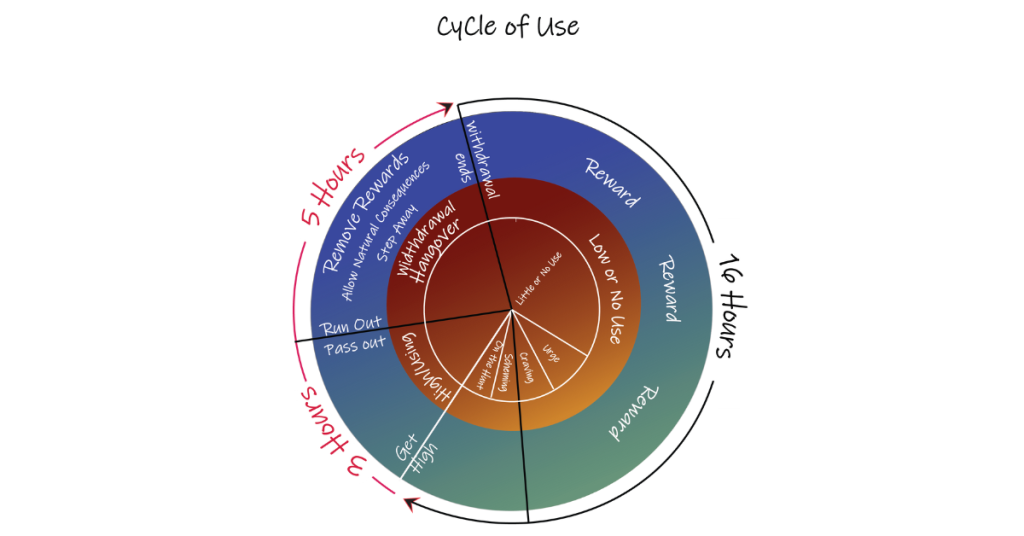
You have all the facts you need: blood spots, soot, spoons in the bathroom, not taking the prescribed suboxone. You clearly know there is use in your house. In accordance with Allies Modules 5 and 6, you’re rewarding positive behavior when they’re not using and removing immediate rewards when they are. This indicates that you know there is use. Your LO is not hiding it so well.
Let’s review a couple of boundary fundamentals, now (we’ll go into this further below). First, your boundaries determine your behavior, not your LO’s. Second, your boundaries are yours, which means they’re also yours to manage. So, To apply this to your situation: your LO is using in your house (which is a boundary of safety for both you and them). What action steps are you going to follow through on?
A way to assertively address the use while giving your LO options could sound something like this:
I’ve observed you nodding off, slurring your words, not taking your suboxone, and sleeping a lot. And I’m really scared and anxious about what is happening. We agreed to no use when living here. It’s not safe for either of us.
“Moving forward, there are a couple of options to choose from in order to live here together. Either (one) A thirty day inpatient treatment with a recovery plan when returning home, or (two) an Intensive Outpatient Program (IOP), taking your suboxone consistently, and attending a couple of mutual aid groups a week while living here. I can help you find either the residential program or the IOP and we can make the calls together if you want, or you could make the calls yourself.
Which one do you want to do?
This is an example of how the conversation could go. Of course, these two options might not be what you and your partner decide to present. You might want to look back at your original agreement and stick to what you had decided would happen if there was use in the house. Or you could get creative and add some new resources that you had not thought of. What’s important in this conversation is to state the facts, stay firm on what needs to happen (regardless of your LO’s response), and present everything with calm, compassion, and understanding.
You do not need them to admit use. You already know that they are, and in any case the burden of proof is not on you. It’s on them to prove they are not. Stating the facts gives you the opportunity to tell them what you know. It’s hard to argue with the facts. This kind of response is assertive without being aggressive and confrontational, but also doesn’t let them avoid what everyone knows is happening.
Be prepared for pushback
They quite probably are not going to respond in a positive way, and they may still continue to deny that they’re using. Cries of, “You never trust me!” “You can’t control me!” and “I’m not using! You’re crazy!” are to be expected, but remember that it’s important not to get pulled into the proof-trap. This is about safety and helping them by managing your boundary. This is the hard part of boundaries: sitting with angst and pressure and still following through, regardless of our LO’s possible behavior.
Write down a mantra or a few phrases you can turn to when your LO pushes back: “Nevertheless, this what we are going with. One of these two plans.” Or, “Regardless, we love you too much to let things stay on the same track. Which plan will work for you?” Or, “That may or may not be. All I have to go on is what I have observed, and we love you too much to let things go any further. We need to know which plan you want to go with by tomorrow, as we need to start making the calls right away.” Have a list of resources ready and offer to help them make the calls.
Knowing that your LO might not respond the way you hope, you ought to have a plan in place for various scenarios. What if they decide to take off and go to a friend’s house? What then? What if they take off and aren’t communicating with you for a bit? How will you handle that?
This is why it is so important to think through boundaries and plans beforehand. Knowing what you can and cannot tolerate is really going to help guide you in creating those boundaries. Now let’s expand on those boundaries’ fundamentals. The key points to remember are:
- You should start with boundaries on narrower, not-too-challenging behaviors first, and build from there.
- The boundaries are yours. They determine your behavior, not your LO’s. They are also for you to manage.
- It is not your LO’s responsibility to follow your boundary. It’s yours. In fact, many people test our limits.
- Boundaries should be set regardless of the outcome of your LO’s behavior.
- You need to figure out in advance what actions steps you’ll take if your LO does not follow the boundaries. Consider this before setting down the boundary, and be prepared for your own angst, ruminating thoughts, and anxiety when following through.
- If you think you won’t be able to follow through on a particular boundary because of safety or because your sanity is in danger, then I would encourage you not to set that boundary in the first place. Instead, find one that you will be able to follow through on.
Maybe when you came to an agreement with your LO, there was no discussion of what would happen if they did start using while living at home? If so, that’s OK. You can adjust the agreement. It’s your boundary, you get to change it up and adjust it if it is not working for your needs
Practice (a lot of it!) makes perfect
It’s just excellent that you’re deploying your CRAFT skills from Modules 4, 5, and 6. Stick with it! There are many nuanced parts of CRAFT that we learn with practice, practice, practice. Getting really good at it takes so much processing and learning. I would also encourage you to continue to reinforce and reward any and all positive steps forward your LO continues to make.
I would also encourage you to make sure to have Narcan (naloxone) at home and give a kit to your LO as well. Everyone should have Narcan on hand regardless of whether they are in active use or not. It’s best to always be as prepared and safe as possible. You can get Narcan at your local pharmacy now without a prescription. Many states have places you can get it for free. You could try a local opioid coalition. Fire departments and sometimes police departments can be very helpful in locating Narcan as well.
I hope that what I wrote in this response is helpful. Setting boundaries and managing them is probably the most difficult thing we need to do for our Loved Ones. These efforts can get so complicated. Our own thoughts and worries can bring on considerable pain. But please know that you have the Allies community to turn to when you need support.
And please keep us updated. We are wishing you progress on your journey with your Loved One.
Laurie MacDougall

















































































LEAVE A COMMENT / ASK A QUESTION
In your comments, please show respect for each other and do not give advice. Please consider that your choice of words has the power to reduce stigma and change opinions (ie, "person struggling with substance use" vs. "addict", "use" vs. "abuse"...)