Benzos, Recovery, And my Own Experience

Our Allies member has concerns about her loved one’s prescription use of benzodiazepines. There seems to be mixed information about the harmful nature of these drugs and she would like to know what evidence points to the use of benzos in a positive light.
This post originally appeared on our Member Site blog, where experts respond to members’ questions and concerns. To learn more about membership, see our Membership Benefits page.
Dominique Simon-Levine looks at both sides of the benzodiazepine argument and shares her own experience
Your son has been taking benzodiazepines for 10 years and wants to continue. His psychiatrist doesn’t see a problem. There have been a “couple” incidents over those 10 years when your son took more than was prescribed but for the most part your son takes this drug safely.
Here is an article that weighs both sides of the benzodiazepine argument. As is typical in this field, there aren’t black and white answers. Outcomes can vary, and careful consideration on a case-by-case basis is emphasized.
The dangers of Benzos of recovery
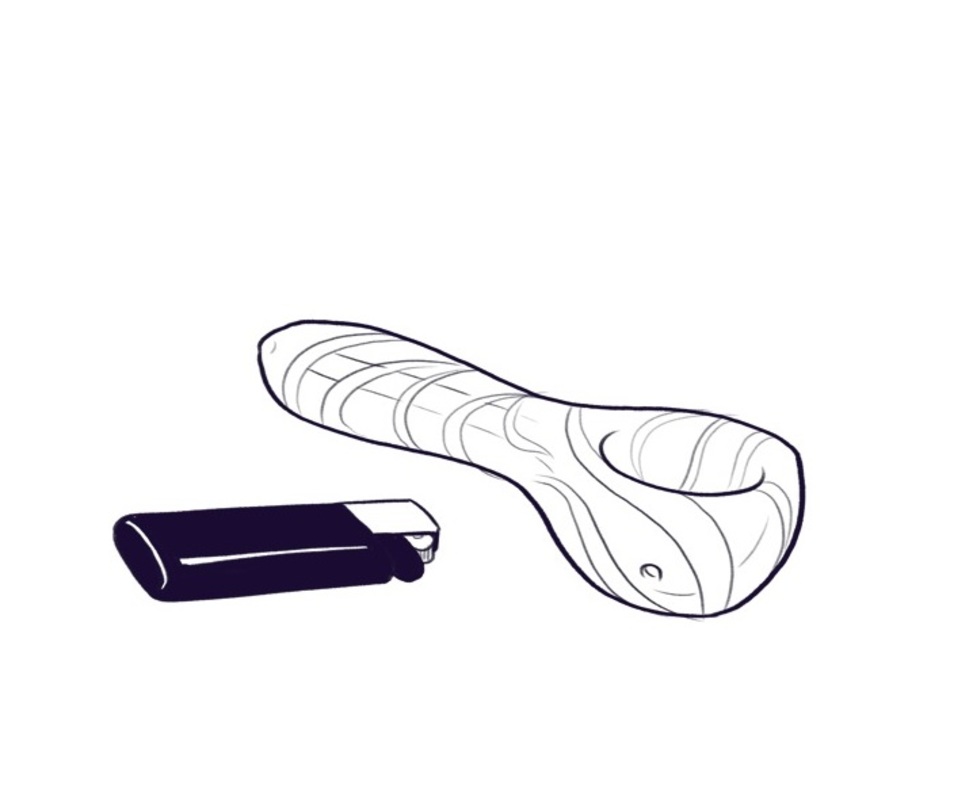
Benzodiazepines help with anxiety and insomnia. (Some of us will remember valium, an early example of a benzodiazepine.) Benzodiazepines are easily addictive and more dangerous when used to boost or extend the high of alcohol or opioids. A high number of deadly opioid overdoses involve the combination of an opioid and a benzodiazepine. People who mix their drugs like this run the risk of more serious respiratory depression than if they had taken only one of the drugs, hence the increased risk of death.
Benzodiazepines are difficult to withdraw from. The symptoms are very uncomfortable: anxiety, restlessness, sleeplessness. Withdrawals can also cause life-threatening seizures, which is why withdrawal needs to be carefully titrated and medically monitored, typically in a detoxification program.
I understand your son’s hesitancy to come off the benzodiazepines and his psychiatrist’s reluctance to take him off. These drugs work well for anxiety and there aren’t a lot of medical alternatives.
Long-term use of benzodiazepines is not well understood. The main concerns are problems with memory. In my own experience, I have successfully taken a small dose of a benzo for over 12 years, without abuse or the need to increase the dose. I do so under the care of an excellent psychiatrist.
On the positive side of recovery
I can tell you benzodiazepines have done more for my recovery than anything else I have ever tried medically. Shortly after starting to take them, my world changed. I felt calmer and safer than I ever had. I could feel the sun on my face. My husband said I had become the person I was always meant to be. I was less irritable, more patient, more open to being in the world. I have complex PTSD and had 14 years of recovery when I started. This is important to note – I was attending peer support meetings, meditating as best I could, exercising, and seeing a therapist regularly. These were all very critical and helpful, but they weren’t sufficient to keep me from anxiety attacks that had me glued to the end of the bed, unable to launch my day.
To this day, I take half the smallest dose and I sleep well. By the way, while benzos are clearly a drug of abuse, I am not alone in taking them in recovery as prescribed over a long period of time. If you took a poll in an AA meeting you would find others who are doing the same as I do. Unlike other drugs I have “sampled” I don’t find that my tolerance builds and that I need more and more to get the same results. The psychiatrist I work with knew this could be the case and was willing to take a chance with me.
Careful monitoring is essential
Whether I was born with anxiety or became anxious as a result of trauma is irrelevant. Navigating it has brought me down some rough paths. Alcohol and opioids worked for a while to settle that internal shaking, the persistent fear, and the feeling that my chest was going to explode. But the consequences of those drugs were also quickly ruining my life.
I will always need to carefully watch what I do to maintain my recovery: peer supports, therapy, psychiatry…. and those are just some of the essentials. Psychiatry for many of us will continue to be a key component in our ability to maintain recovery and to live a more quality life.
Perhaps this will help to fill out some more of the background as you consider your son’s situation. Should he choose to stay on the prescription, careful monitoring by his psychiatrist is clearly of great importance. But as a stand-alone for someone with addiction, it becomes a slippery slope. He needs to seek out and engage with a constellation of supports including peer recovery groups and other activities that help advance his recovery work. I hope this is helpful for you both. Thanks for writing in with this important question.
Since 2003, Allies in Recovery has addressed substance abuse in families by providing a method for the family to change the conversation about addiction. We use Community Reinforcement & Family Training (CRAFT), a proven approach that helps the family unblock and advance the relationship towards sobriety and recovery and to engage a loved one into treatment. Learn about member benefits by following this link.